For years the McClung lab has taken advantage of mouse, cell culture and rat models to better understand how circadian genes function at a molecular level in multiple brain regions to control mood, reward, anxiety, impulsivity, and cognitive control. We use state of the art techniques to manipulate expression and rhythms in these key circadian factors within specific cell types and brain regions to determine how this impacts cellular activity, electrophysiology, and behavior.
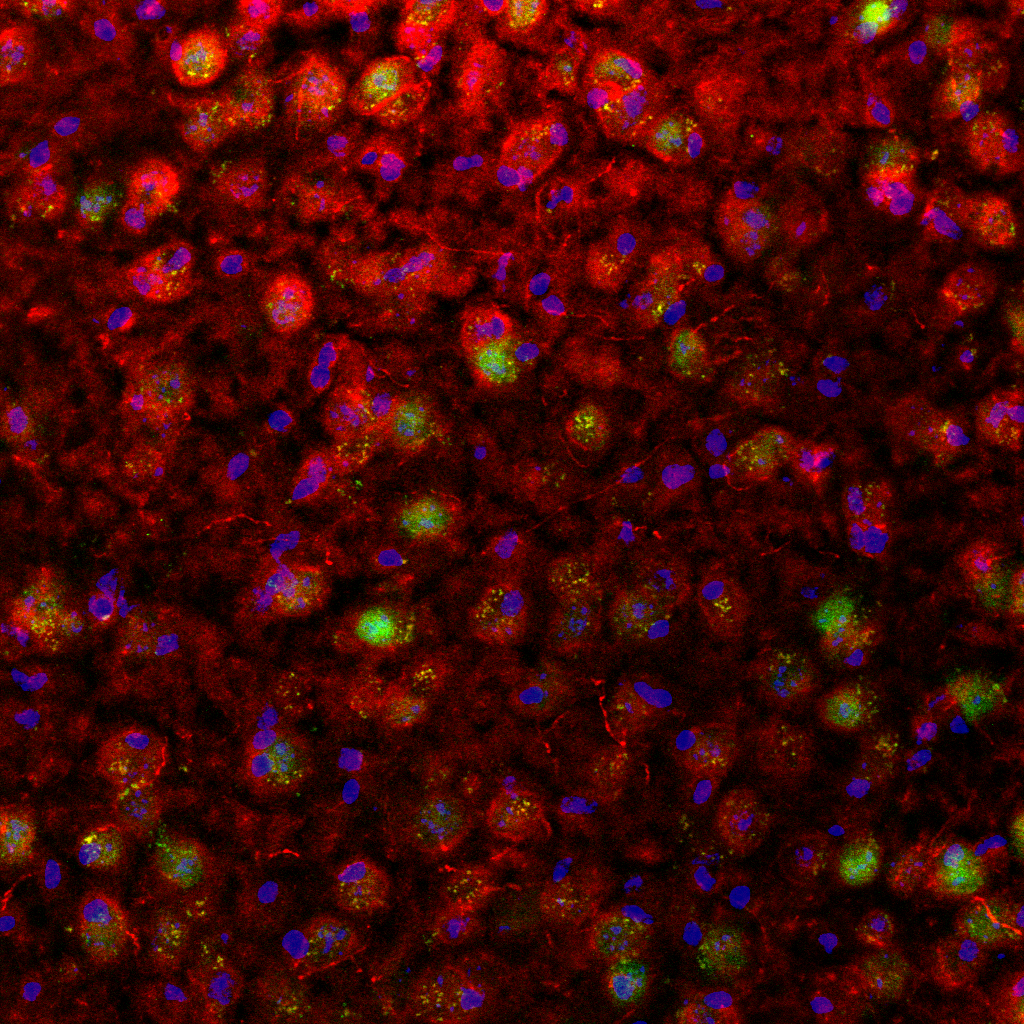
Through these studies we have identified some key interactions between cellular metabolic factors and circadian protein function, indicating a bi-directional relationship between molecular rhythms in gene expression in the nucleus and mitochondrial and antioxidant function in the rest of the cell (Logan et al., 2019). For example, we discovered key functions of the molecular clock in astrocytes in the nucleus accumbens in the regulation of lactate production and reward (Becker-Krail et al., 2022).
We also use optogenetic, chemogenetic and other approaches to better understand the importance of rhythmic activity patterns in multiple brain circuits, and how either increased communication or disruptionbetween cells in the master pacemaker of the brain, the SCN, impacts psychiatric disease-related behavior (Vadnie et al., 2021).
 Circadian rhythm and sleep disruptions are a defining feature of psychiatric disorders like bipolar disorder (BP), schizophrenia (SCZ) and major depressive disorder (MDD). These disruptions to normal rhythmicity include altered sleep/wake cycles, diurnal patterns of hormone levels, and circadian gene expression in peripheral samples. Moreover, disruptions to the normal sleep/wake cycle often precipitate mood and psychotic episodes and may contribute to deficits in cognitive function. However, the molecular rhythm changes that occur in human brain in subjects with psychiatric diseases remain largely unknown.
Circadian rhythm and sleep disruptions are a defining feature of psychiatric disorders like bipolar disorder (BP), schizophrenia (SCZ) and major depressive disorder (MDD). These disruptions to normal rhythmicity include altered sleep/wake cycles, diurnal patterns of hormone levels, and circadian gene expression in peripheral samples. Moreover, disruptions to the normal sleep/wake cycle often precipitate mood and psychotic episodes and may contribute to deficits in cognitive function. However, the molecular rhythm changes that occur in human brain in subjects with psychiatric diseases remain largely unknown.
With the measurement of rhythmic gene expression in the human brain now possible, our group and others have demonstrated molecular rhythmicity on a genome-wide scale by employing a “time of death” analysis to order postmortem human brain samples around a 24-hour cycle. One of the first studies using this technique was done by Li et al. and found that MDD subjects had major disruptions in molecular rhythms across six different brain regions, including prefrontal cortex (PFC) area 46 and subgenual cingulate (SGC) area 25, compared with comparison subjects. Using the same approach in a cohort of 146 control subjects (ranging in age from 16 to 96 years), we found that two PFC regions exhibited highly significant patterns of rhythmic gene expression (Chen et al., 2016).
Moreover, we found that normal aging was associated with a significant loss of rhythmicity in several transcripts and a surprising gain of rhythmicity in others. We have gone on to publish multiple studies which define the differences in rhythmic patterns of gene expression across cortical and striatal regions both control subjects and subjects with major psychiatric disease. We have found that subjects with schizophrenia have a surprising gain of rhythmicity or “circadian reprogramming” in a number of transcripts associated with mitochondrial function in the PFC (Seney et al., 2019). We have also identified a number of changes in gene expression rhythms in striatal regions in subjects with psychosis (Ketcheisin et al., 2022). These data have provided unprecedented insight into the way the human brain functions over the day/night cycle and how changes that occur to these rhythmic patterns may contribute to the development of psychiatric disorders.
 Substance use disorders (SUD) are a major public health problem that impact millions of people and their families. The factors that contribute to SUD vulnerability, as well as the transition from drug use, abuse, and to SUD remain unclear. We know that the reward value for alcohol and drugs of abuse varies by time of day. For example, for most individuals, the desire to drink wine or beer is very different at 6:00am compared to 6:00pm.
Substance use disorders (SUD) are a major public health problem that impact millions of people and their families. The factors that contribute to SUD vulnerability, as well as the transition from drug use, abuse, and to SUD remain unclear. We know that the reward value for alcohol and drugs of abuse varies by time of day. For example, for most individuals, the desire to drink wine or beer is very different at 6:00am compared to 6:00pm.
There is a normal, time of day dependent, rhythm in the reward value for these drinks and this rhythm is protective against SUD. In fact, one of the key factors that is used to evaluate the transition to addiction is the loss of diurnal rhythmicity in reward value (e.g., the desire to drink alcohol in the morning). In addition to alcohol, when the reward circuitry has been hijacked by chronic exposure to other drugs of abuse, circadian rhythms in reward circuitry are lost, and these rewards overtime develop equal value at any time of day. Genetic factors (circadian gene variations) also contribute to reduced rhythms in reward at baseline, prior to any drug exposure, and increased SUD-related vulnerability. Indeed, mice with circadian gene mutations show greater drug self-administration and a loss in the normal diurnal rhythm in this behavior (Ozburn et al.,2012; DePoy et al.,2021). By determining the molecular and cellular mechanisms that underlie natural diurnal rhythms in reward, we can potentially help prevent the transition between use to SUD."
Dr. McClung is the overall director and PI of Project 3 of the NIDA Research Center of Excellence (P50) entitled, Center for Adolescent Reward, Rhythms and Sleep (CARRS). Adolescence is a vulnerable time for substance abuse. This risk reflects the heightened reward system of adolescence, which is found regardless of cultural upbringing or home environment, relative to both adults and children. In addition, genetic, social, and environmental factors influence the amount of sleep and circadian rhythm misalignment experienced by the adolescent brain.
The primary goal of CARRS is to integrate human and rodent studies to understand the impact of adolescent sleep and circadian rhythm changes (both biologically and environmentally induced) on reward circuitry and SUD-relevant outcomes. We will use experimental manipulations to further examine how sleep and circadian rhythms affect reward function and substance use (SU)-related outcomes, with an aim to develop novel prevention or intervention strategies.
The central hypothesis of the Center is that adolescent development acts on underlying sleep and circadian traits to modify homeostatic sleep drive, circadian phase, and circadian alignment, which in turn impact cortico-limbic functions critical to substance use risk (e.g., reward and cognitive control). We further hypothesize that manipulation of sleep and circadian factors during adolescence will alter reward sensitivity, cognitive control, and the risk for future substance use ad abuse. In turn, abuse of drugs will also impact the circadian, reward and sleep systems creating a vicious cycle. Interventions that help stabilize the circadian and sleep systems or reduce the damage done by these disruptions may be protective against substance abuse in vulnerable individuals.
The overall goals of the center are to 1) Determine the role of sleep and circadian rhythms in reward sensitivity and substance use (SU) in adolescence 2) Conduct translational research aimed at development of interventions to reduce risk in at-risk individuals 3) Partner with other Centers and the addiction research community to inform and complement ongoing research 4) Provide training and education on sleep circadian rhythms, and substance use.
 The McClung lab is actively involved in research aimed at developing novel therapies for psychiatric and other disorders through manipulation of the circadian clock. We know, for example, that mood episodes in bipolar disorder are often precipitated by changes to the sleep/wake schedule and that stabilization of daily rhythms can prevent these episodes. Furthermore, treatments for this disorder including lithium and valproic acid are known to enhance and strengthen molecular clock function and this could underlie many of their mood stabilizing effects.
The McClung lab is actively involved in research aimed at developing novel therapies for psychiatric and other disorders through manipulation of the circadian clock. We know, for example, that mood episodes in bipolar disorder are often precipitated by changes to the sleep/wake schedule and that stabilization of daily rhythms can prevent these episodes. Furthermore, treatments for this disorder including lithium and valproic acid are known to enhance and strengthen molecular clock function and this could underlie many of their mood stabilizing effects.
We have found, for example, that a molecule that targets molecular clock function through Casein Kinase 1 improves manic-like behavior in a mouse model of bipolar disorder (Arey et al., 2012). The identification of pharmacotherapies that target the circadian system should provide a more direct impact on mood without unwanted side effects.
We are also interested in identifying ways to help entrain and shift circadian rhythms for help with jet lag, shift work, and to help teens with an extreme evening preference become more in line with early morning school start times. Our goal is to perform translational research that takes basic research discoveries to the clinic.
